Measurement-Based Care (MBC) relies on tools like PHQ-9 and GAD-7 to track symptoms and improve mental health treatments. However, MBC only works if patients actively participate by attending appointments and completing assessments. Without this involvement, data gaps occur, making it harder for clinicians to adjust treatments and identify worsening conditions.
Key points from the article:
- Missed Appointments: Skipping sessions leads to fewer data points, making it hard to monitor progress and adjust care.
- Incomplete Surveys: Low completion rates for tools like PHQ-9 create unreliable data, delaying necessary interventions.
- Engagement Improves Outcomes: Patients involved in reviewing their data feel more connected to their care, which strengthens the therapeutic relationship and improves results.
Solutions to boost engagement:
- Review Data Together: Discussing survey results during sessions builds trust and shows patients how their input shapes care.
- Tailor Assessments: Aligning tools with patient goals makes them more relevant and encourages participation.
- Explain Data Use: Transparency about how data drives treatment decisions increases trust and compliance.
Tools like CaredFor assist by automating appointment reminders, simplifying data collection, and fostering community support, helping patients stay engaged and improving MBC outcomes.
How Poor Patient Engagement Breaks MBC Programs
Missed appointments and incomplete assessments disrupt the flow of data collection that’s critical for Measurement-Based Care (MBC). Without steady participation from patients, clinicians lose the ability to monitor progress, catch signs of worsening conditions, and make evidence-based adjustments to treatment plans. One of the clearest examples of this disruption is missed appointments, which we’ll explore next.
Missed Appointments Create Data Gaps
Every skipped session means one less data point. When patients miss appointments, providers are unable to complete the vital “Share” and “Act” phases of MBC – steps where they review assessment scores with patients and collaboratively modify treatment plans.
These gaps can lead to clinical inertia, where ineffective treatments continue simply because there’s no objective data to guide changes. Tools like progress graphs, often shared during sessions, help patients connect their symptoms to the skills they’re learning. Without these visual aids, patients miss out on valuable feedback, which can weaken their commitment to the process and make them less likely to stay engaged in the future.
Low PHQ-9 Completion Rates Produce Unreliable Data
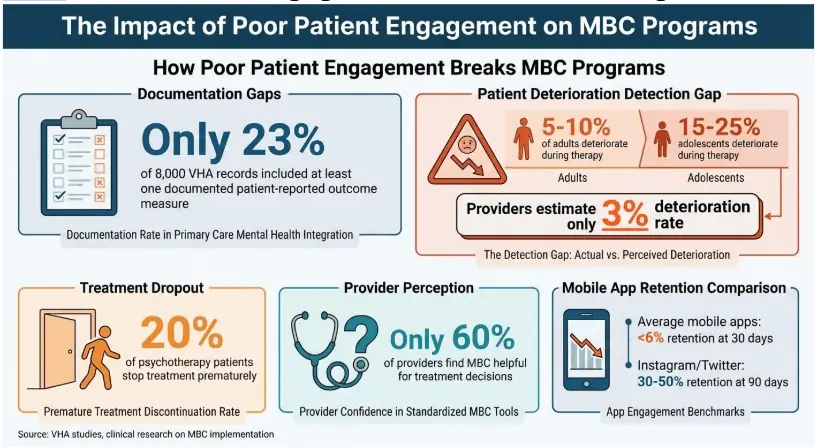
Inconsistent PHQ-9 survey completions result in unreliable data, which can distort the true effectiveness of clinical interventions. Instead of reflecting the intended treatment approach, the data often mirrors irregular usage. For instance, a survey of the VHA’s Primary Care Mental Health Integration program revealed that only 23% of 8,000 records included documentation of at least one patient-reported and validated outcome measure.
Without dependable longitudinal data, clinicians struggle to identify patients whose conditions are worsening. Research shows that 5% to 10% of adults and 15% to 25% of adolescents actually deteriorate during therapy, but providers often estimate this rate at just 3%. This gap in awareness means patients in need of urgent intervention may remain on ineffective treatment plans until their condition reaches a critical point. Regular engagement is essential to avoid such scenarios and maintain clinical compliance, as discussed below.
Why Engagement Determines Clinical Compliance
Consistent participation not only ensures adherence to treatment protocols but also strengthens the therapeutic relationship. Patients who review self-reported scales during sessions often feel more involved in their care decisions. This collaborative approach is especially important for racial and ethnic minority patients, who are more likely to drop out of therapy.
Dr. Andrew D. Carlo, from the Meadows Mental Health Policy Institute, emphasizes the importance of early intervention:
MBC facilitates early identification that a patient is still symptomatic and can prevent the clinical inertia of continuing ineffective treatments.
These challenges highlight why patient engagement is the cornerstone of successful outcomes. Research involving 21,000 patients demonstrated that MBC reduced symptoms across all case types, with the most significant improvements seen in patients who were “not on track” for recovery. However, these benefits depend entirely on consistent patient involvement in the data collection process.
How to Increase Patient Engagement in MBC
Getting patients more involved can breathe new life into struggling Measurement-Based Care (MBC) programs. When clinicians make an effort to include patients in the process, completion rates go up, and the data becomes dependable enough to guide treatment decisions. By working with patients during sessions, tailoring assessments to their needs, and being transparent about how the data is used, clinicians can turn MBC into a true partnership in care.
Review Patient Data Together During Sessions
Sitting down with patients to go over their reported measures builds trust. It shows that their input directly influences care decisions. For instance, at the Veterans Health Administration, clinicians who took the time to explain MBC over several visits noticed a clear boost in patient engagement and cooperation. Why? Because patients began to understand why they were filling out assessments and how their answers shaped their treatment. Jessica Barber, PhD, from Yale University School of Medicine, puts it this way:
Using data forms as an integral part of treatment operationalizes the therapeutic alliance by inviting patients to repeatedly and regularly let us know what they’re thinking.
When clinicians discuss tools like PHQ-9 scores during appointments, patients can see the direct link between their symptoms and any changes to their treatment plan.
Choose Measures That Match Patient Goals
After reviewing data together, using measures that align with a patient’s personal goals can take engagement to the next level. Standardized assessments often feel like meaningless paperwork, but personalized measures focus on tracking what matters most to the patient. Interestingly, only 60% of providers find MBC helpful for making specific treatment decisions, largely because standardized tools don’t always reflect individual patient needs. A better approach combines these standardized tools with patient-specific goals. When assessments reflect a patient’s unique situation and preferences, engagement naturally improves. This personalization ensures that patients don’t feel like they’re just filling out forms – they see how the process connects directly to their recovery.
Explain How Patient Data Informs Treatment
Once measures are tailored to patient goals, being clear about how the data drives treatment decisions is key to maintaining engagement. Transparency about data use not only boosts completion rates but also builds trust. Patients need to see that their PHQ-9 scores or other assessments are actively shaping their care. At Yale New Haven Health System, clinicians adopted a “Collect, Share, Act” framework. This meant working with patients to choose the right measures, reviewing results together, and using the data to guide treatment decisions. The result? Better patient engagement and satisfaction. When patients see their input leading to real changes in their care, they’re much more likely to stay consistent with future assessments.
Empower Behavioral Health with Tailored SolutionsDiscover cloud-based EHR, HCM, and Patient Engagement platforms designed to streamline workflows, enhance workforce management, and improve client outcomes for behavioral health organizations.Explore Solutions |
How CaredFor Improves Patient Engagement and MBC Results

Even the best clinical strategies can fall short without the right technology to keep patients engaged. CaredFor steps in by automating communication, simplifying data collection, and strengthening the connection between patients and care teams.
Automated SMS Reminders and Personalized Messages
Text messages are a powerful tool for cutting through distractions that can lead to missed appointments or incomplete assessments. With CaredFor, automated SMS reminders are tailored to support “Care Journeys” – personalized treatment plans designed to help patients stay aligned with their clinical goals. These messages go beyond generic reminders, adapting to each patient’s specific stage of treatment.
Research indicates that around 20% of psychotherapy patients stop treatment prematurely. Dylan Souza, Vice President of Marketing at ContinuumCloud, highlights the importance of keeping patients engaged:
When patients feel invested in their treatment, they are more likely to engage in shared decision making, adhere to mental health services, keep appointments, and follow through with health practices recommended by their trusted health professionals.
CaredFor’s HIPAA-compliant auto-responses ensure quick communication, while clinicians can track metrics like cancellation-to-reschedule ratios to identify patients who might need extra support. This seamless communication also makes data collection much easier.
Secure and Easy Access to PHQ9 and Other Measures
CaredFor simplifies the process of collecting patient-reported outcome measures like PHQ-9 scores by offering a secure platform accessible via mobile devices or on-site in waiting rooms. After appointments, automated surveys are sent to patients, gathering important data without adding extra work for the clinical staff. Plus, the platform integrates directly with the organization’s EHR, giving clinicians real-time data to discuss during sessions.
Online Community Tools for Long-Term Engagement
Keeping patients engaged over the long term requires more than just reminders. CaredFor fosters a sense of community by involving families, caregivers, and alumni in the care process. Through peer support and moderated social media features, the platform helps reduce the feelings of isolation often experienced during behavioral health treatment. Studies have shown that social network support can boost engagement and alleviate symptoms.
This community-focused approach complements CaredFor’s communication and data tools by encouraging ongoing involvement. Alumni features allow patients who’ve completed treatment programs to stay connected, offering mentorship to newer patients while continuing to support their own recovery. Considering that average 30-day retention rates for mobile apps hover below 6%, and even major apps like Instagram and Twitter only see 30–50% retention after 90 days, CaredFor’s ability to maintain patient engagement well beyond these averages is notable. Clinicians can also track community engagement data through the integrated EHR, gaining real-time insights into patients’ social support and activity levels.
Conclusion
Measurement-based care (MBC) struggles when patients aren’t actively involved. Without their participation, programs face issues like incomplete data, missed appointments, and unreliable tracking, making it difficult to spot when treatments fall short. This highlights the importance of patient-reported data – but it only works when patients are consistently completing their assessments. The challenge lies in creating systems that truly engage patients.
The solution? Build a framework where patients clearly see their role in shaping their care. When they review progress graphs during sessions, use measures tied to their personal goals, and see how their input directly influences treatment decisions, they transition from passive participants to active collaborators. This collaboration strengthens the therapeutic relationship, which is a key factor in achieving better outcomes.
Key Takeaways
The success of MBC depends on strong patient engagement. The “Collect, Share, Act” framework only works when patients reliably attend sessions, complete assessments, and engage in meaningful discussions with their clinicians. Achieving this level of engagement requires strategies like personalized reminders, easy access to assessments, and fostering a sense of community.
CaredFor addresses these challenges head-on by integrating automated communication, streamlined data collection, and community support into one platform. With personalized text reminders tailored to each patient’s journey, mobile-friendly access to assessments, and peer connection opportunities, patients are much more likely to stay engaged throughout their treatment.
Request a Demo of CaredFor
Ready to enhance patient engagement and improve MBC outcomes? CaredFor can help. Schedule a demo to explore how our platform simplifies the entire engagement process – from appointment reminders to real-time outcome tracking – while easing the workload for your clinical team.
FAQs
Why is patient engagement essential for the success of Measurement-Based Care?
However, when engagement drops, the flow of data is disrupted. This makes it challenging to monitor progress and fine-tune treatment plans. In short, without active patient participation, MBC falls short of its ability to deliver improved health outcomes.
How can we boost patient engagement in measurement-based care (MBC) programs?
Effective communication plays a big role here. Clearly explain how completing assessments contributes to more personalized care and better outcomes. Streamlined digital tools with features like one-click surveys, auto-save, and offline access can help remove common barriers. Adding milestone-based content – like celebrating progress – can reinforce positive habits. Even small rewards, like progress badges or gift cards, can keep patients motivated and make MBC feel like a natural part of their care journey.
How does the CaredFor platform improve patient engagement in mental health care?
Through a combination of an intuitive app and advanced analytics, patients can view their scores, access customized educational resources, and securely communicate with their care team. This approach empowers patients to take an active role in their care, leading to fewer missed appointments, better data quality, and stronger treatment outcomes. By placing engagement at the heart of mental health care, the platform supports more effective and connected care experiences.




